By Isabella Backman
New Haven, Nov 23, 2025.- Yale School of Medicine (YSM) researchers have made key breakthroughs in understanding how to treat fibrotic diseases such as scleroderma and graft-versus-host disease.
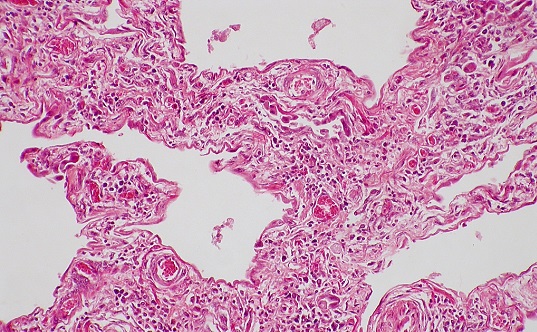
Fibrotic diseases are a group of conditions—often autoimmune—characterized by excessive tissue scarring. They can drastically hinder patients’ quality of life, and in some cases, they can be life-threatening—fibrosis contributes to approximately 45% of all deaths in developed nations. However, there are no effective treatments.
Now, in a study published in Blood, researchers have developed a monoclonal antibody that is showing promise as a new therapy for patients. And in a Nature Communications study, the same team discovered a signaling pathway that may be mediating fibrosis and could be a target for future therapies.
“Treatments for fibrosis are an enormously unmet need,” says Richard Flavell, PhD, Sterling Professor of Immunobiology at YSM and co-principal investigator of the studies. “Better understanding these conditions will likely yield new medicines to help patients.”
New therapeutic antibody mitigates fibrosis
Previous research has linked the upregulation of a protein called epidermal growth factor receptor (EGFR)—which helps control how cells grow and multiply—with fibrotic diseases. Typically, this protein helps promote wound healing. But when it becomes overactivated, it can produce excessive scar tissue associated with fibrosis.
In 2022, the YSM researchers found that skin samples from patients with scleroderma—a rare autoimmune disease that causes fibrosis of the skin and sometimes internal organs—had increased levels of epiregulin, a signaling molecule that binds to EGFR. They hypothesized that more epiregulin could be driving the overactivation of EGFR, leading to fibrosis in scleroderma. To test this idea, they used an antibody to target and reduce epiregulin in animal models and found that it reversed fibrosis.
Based on these findings, in their latest study, the team developed a new human anti-epiregulin therapeutic antibody and tested its ability to mitigate graft-versus-host-disease, a complication of stem cell or bone marrow transplants in which donor immune cells attack the body and, in some cases, cause fibrosis. First, the researchers compared single-cell RNA sequencing data from patients with scleroderma and graft-versus-host disease to identify the shared mechanisms driving fibrosis in both diseases and they confirmed that upregulated epiregulin was a common pathology.
“What really stood out was that the epiregulin signal, like we had seen before in scleroderma, was really highlighted in patients with this fibrotic graft-versus-host disease,” says Ian Odell, MD, PhD, assistant professor of dermatology at YSM and co-principal investigator of the studies.
Then, the team tested their anti-EREG antibody in humanized mouse models and skin biopsies from patients and found that inhibiting epiregulin reduced biomarkers associated with fibrosis. These findings suggest that the therapeutic antibody could be a promising new therapy for patients with various types of fibrotic conditions.
In future studies, the researchers plan to test the therapy in other fibrotic diseases such as lupus and hidradenitis suppurativa.
Researchers identify pathway underlying fibrosis
In a second recent study, the researchers aimed to further understand mechanisms that differentiate fibrotic and non-fibrotic skin diseases. The team compared single-cell RNA sequencing data from seven different inflammatory skin diseases. Some of the diseases, like atopic dermatitis and psoriasis, were associated with redness and scaling, but not fibrosis. They also analyzed data from patients with fibrotic diseases such as scleroderma, graft-versus-host disease, and lupus.
Their analyses revealed that fibrotic diseases were associated with greater activity of a protein called STAT1 in fibroblasts, the key cell type that’s hyperactivated in fibrotic diseases. To better understand how STAT1 interacts with the EGFR signaling pathway to drive fibrosis, the researchers developed mouse models that lacked STAT1. When the team activated EGFR, they found that mice without STAT1 showed less fibrosis compared to regular animal models.
“If we activate EGFR by inducing injury when there’s no STAT1 present, none of the fibrotic genes are activated,” says Odell.
The researchers conducted further experiments on cultured fibroblasts in vitro which confirmed that STAT1 was required for the onset of fibrosis.
Current therapies for skin diseases include Janus kinases (JAK) inhibitors, which target the JAK-STAT pathway. Previous research shows that the activation of JAKs can trigger activity of STAT proteins like STAT1. While JAK inhibitors can successfully treat skin diseases like atopic dermatitis and psoriasis, they are less effective in mitigating fibrosis.
The current study shows that EGFR signaling can activate STAT1 independent of JAKs, which could explain why JAK inhibitors don’t work as well for fibrotic diseases. This EGFR-STAT1 pathway is a promising new target for potential therapies, the researchers say.
Importantly, the upregulation of epiregulin activation of EGFR-STAT1 pathway isn’t always active—it’s only switched on under specific conditions such as the presence of injury or inflammation. “These are not targets required for living your daily life—we’re not expecting significant side effects by inhibiting them,” says Odell. “We’re expecting a very safe profile.”
The new studies highlight two promising therapeutic avenues for treating fibrotic diseases. The researchers are optimistic that they will lead to new tools that will greatly improve patients’ quality of life. “There’s a lot of hope for the future,” Flavell says.